Core Knowledge: Talus Fractures
23/10/13 07:06 Filed in: Core Knowledge | Wednesday Blog

Today’s Wednesday Blog looks at fractures of the Talus, a topic that has featured as a clinical question in previous ST3 Orthopaedics interviews.
Background
- The talus articulates with the calcaneum, tibia and navicular bones to form three joints: the subtalar joint, the tibiotalar joint and the talonavicular joint.
- The talus is usually fractured by a high energy injury with forced dorsiflexion and an axial load.
- 50% of talus fractures are fractures of the talar neck with the reminder being fractures to the body, head or lateral or posterior processes.
- Fractures are associated with dislocations of the above joints which need reducing in the acute setting.
Anatomy

The talus is supplied by three arteries:
- Posterior tibial artery
- via artery of tarsal canal (dominant supply)
- supplies majority of talar body
- deltoid branch of posterior tibial artery
- supplies medial portion of talar body
- may be only remaining blood supply with a displaced fracture
- Anterior tibial artery
- supplies head and neck
- Perforating peroneal artery via artery of tarsal sinus
- supplies lateral head and neck
- The talus receives a retrograde blood supply and it’s body is thus at risk to AVN in a similar manner to the femoral head and scaphoid.


Classification
- Hawkins classification correlates position of talar neck fractures with their subsequent risk of AVN.
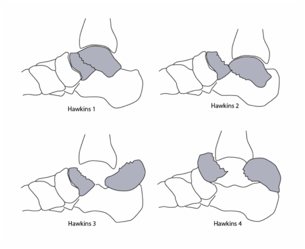
Hawkins I: Undisplaced
Hawkins II: Subtalar dislocation
Hawkins III: Subtalar + Tibiotalar dislocatio
Hawkins IV: Subtalar + Tibiotalar + Talonavicular dislocation
Risk of AVN
- I 0-13%
- II 20-50%
- III 20-100%
- IV 70-100%
Imaging
AP + Lateral radiographs of foot and ankle
CT is gold standard to assess fracture pattern
XRs at 6-8 weeks post reduction will demonstrate a positive Hawkins Sign if blood supply is intact. An absent Hawkins sign is evidence of osteonecrosis.

Hawkins sign is lucency in the subchondral bone on XR indicating active bone resorption and thus an intact blood supply.
Management
As fractures are high energy patients should be resuscitated using ATLS protocols with documentation of neurovascular status.
Reduce
- Dislocations of the joints around the talus should be acutely reduced.
- Reduction manoeuvres are similar to ankle dislocation reduction with toes lifted, knee flexed, foot plantar flexion and inline traction with inversion or eversion depending on the direction of dislocation.
- This may be attempted in the emergency department but if this is not successful may necessitate theatre with image intensifier and then plaster.
- Approximately 30% of fractures will not reduce closed and require open reduction and internal fixation on a consultant operating list.
- CT should be performed post reduction to assess fracture patterns.
Stabilise
- Hawkins I (undisplaced) fractures may be managed conservatively in plaster NWB for 6 weeks.
- Hawkins II-IV fractures require open reduction and internal fixation with mini fragment screws and small fragment plates through medial and lateral incisions, followed by NWB for 6 weeks.
- The medial incision for ORIF is made between tib post and tib ant
- The lateral incision is made in line with the 4th MT
- In elderly or diabetic patients with severe dislocation and comminution fusion with a hindfoot nail allows for immediate post-op mobilisation
Complications
The three main complications following fracture are:
- Avascular necrosis
- Post-traumatic arthritis (30-50%)
- Varus malunion (25%)

